Medico-Legal Cases (MLC) and Post-mortem Procedure in Cases of Death in Hospitals: Legal Framework, Process, and Remedies
Abstract
This writeup explores the procedural and legal framework governing Medico-Legal Cases (MLC) in the event of a patient’s death within a hospital setting. It outlines the responsibilities of hospitals, the role of law enforcement, the legal necessity and conduct of post-mortem examinations, and the options available to family members if they are dissatisfied with the outcome. This study incorporates recent case laws and statutory provisions, providing a practical and legal guide for handling such sensitive situations.
Introduction
In our daily lives, we often see doctors as professionals who treat illnesses and injuries. However, there are situations where their role goes beyond just providing medical care. When a person is injured or dies under suspicious, violent, or unnatural circumstances—such as in an accident, assault, suicide, or poisoning—the case becomes both a medical and legal matter. These are called medico-legal cases (MLCs). In such cases, doctors are responsible not only for treating the patient but also for carefully documenting injuries, collecting evidence, and informing the police. Their medical reports often become important pieces of evidence in court. Understanding what medico-legal cases are helps us appreciate the critical role doctors play in both saving lives and supporting justice.
What is Medico-legal cases?
A medico-legal case (MLC) refers to any situation where a medical examination or treatment has legal implications. In such cases, a doctor is not only responsible for providing medical care but also for documenting injuries, findings, and other observations that may serve as legal evidence. These cases often arise when the circumstances surrounding an injury or illness suggest a possible violation of law or the need for legal investigation. Common examples of medico-legal cases include road traffic accidents, physical assaults, suspected poisoning, suicide attempts, sexual assaults, burn injuries, and cases of unnatural or suspicious deaths.
Suppose, A 28-year-old man, Ramesh Kumar, is brought to the emergency department late at night with head injuries, bruises, and signs of trauma. He tells the doctor that he was attacked by three men with sticks while returning home from work. Given the nature of the injuries and the circumstances, the attending medical officer immediately registers the case as a medico-legal case (MLC). The patient is given necessary treatment, and the police are informed.
In some instances, even workplace injuries or cases of child abuse may fall under this category. When handling an MLC, a doctor is legally and ethically required to treat the patient first and then notify the police or relevant legal authority. Accurate documentation, preservation of evidence, and maintaining confidentiality are crucial aspects of managing such cases. The medical report provided by the doctor may later be used in court proceedings, and the doctor may be called upon to testify as a witness. Medico-legal cases play a vital role in bridging healthcare and law, ensuring that justice is served while safeguarding the rights and responsibilities of both patients and medical professionals.
Even the Karnataka High court in the case called Smt. Reshma W/O Ramesh Sutar v. Shri Amool Laxman Ukirde (2020) examined what qualifies as an MLC. It clarified that:
“Any case of injury or ailment where the attending doctor … considers that investigation by law enforcement agencies is warranted … he shall treat the said case as Medico Legal Case … immediately … inform the jurisdictional police as provided under Section 39 of Cr.P.C.”
In another case called Parmananda Katara v. Union of India (1989), the Court laid down a fundamental principle: “when a person requires urgent medical treatment, all other considerations must yield to the patient’s right to life”. It held that doctors—even in public or private hospitals—must provide immediate medical care in emergencies (including medico-legal cases) before notifying the police or seeking permission
Medico-Legal Cases (MLCs) involve injury or death where legal investigation is mandatory, such as in cases of accidents, suicides, homicides, or unexplained medical conditions. When a patient dies in a hospital under MLC circumstances, a specific legal process is triggered to ensure transparency, accountability, and justice.
Format for Intimation of MLC
INTIMATION OF MEDICO-LEGAL CASE (MLC)
From:
Hospital Name & details:____________
Pin: __________
To,
The Sub-Inspector of Police,
__________________________ Police Station
Subject: Intimation Regarding a Medico-Legal Case
Sir/Madam,
This is to inform you that a patient named ________________________, ☐ Male ☐ Female, aged _____ years, ☐ Son ☐ Daughter ☐ Wife of ________________________, resident of ___________________________________________, has been brought to the ☐ Emergency ☐ OPD ☐ Ward, at _____ AM/PM on (date): ________________________,
alleged to have been involved in the following incident:
(Brief history and condition of the patient):
The incident is reported to have occurred at ________________on (date): ____________ at _____ AM/PM.
Attending Doctor’s Name & Designation: _________________________
Registration Number: _________________________
Signature of Doctor: _________________________
Date & Time: _________________________
The patient is currently being treated as:
☐ Outpatient ☐ Inpatient in Ward No. __________ / Emergency______________
This information was also communicated via telephone to ________________________ (Name of Police Officer), Buckle No. __________ of ________________________ Police Station on (date) __________ at _____ AM/PM.
Kindly do the needful.
Date: _________________________
Time: _________________________
Yours faithfully,
Signature: _________________________
Name: _________________________
Designation (Security Personnel/Doctor): _________________________
Death in Medico-legal case
In the medico-legal case (MLC), if a person dies in the hospital, It is the duty of the hospital that the police must be informed immediately, Death certificate should not be issued in Medico-legal cases and body must be sent for Medico-legal autopsy after filling the appropriate format.
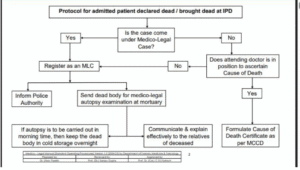
Procedure when the death happened in MLC
Format in case of death happened
INTIMATION OF DEATH IN A MEDICO-LEGAL CASE
From:
Hospital Name & details:____________
Pin: __________
To,
The Sub-Inspector of Police,
(Name and Address of Police Station)
Subject: Information Regarding Death in a Medico-Legal Case
Sir,
This is to inform you that the patient named ________________________,
☐ Male ☐ Female, aged _____ years,
☐ Son ☐ Daughter ☐ Wife of ________________________,
resident of ________________________________________,
was admitted to this hospital in Ward No. / OPD / Emergency: ________________________
on (date): __________ at _____ AM/PM as a Medico-Legal Case, and has expired on (date): __________ at _____ AM/PM.
OR
was brought dead to this hospital on (date): __________ at _____ AM/PM.
The information of medico-legal registration was already sent on (date): __________
at _____ AM/PM.
The apparent cause of death is:
Kindly take necessary action as per protocol.
Date: _________________________
Time: _________________________
Yours faithfully,
Signature: _________________________
Name: _________________________
Designation: _________________________
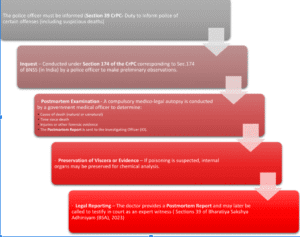
Medico Legal Autopsy in MLC
A medico-legal autopsy (also called a forensic autopsy) is a systematic post-mortem examination conducted in cases of medico-legal deaths, where the cause of death is uncertain, suspicious, or requires legal clarification. Unlike clinical autopsies (done with family consent for medical understanding), medico-legal autopsies are mandatory and performed under legal authority—usually requested by the police or magistrate.
Purpose of Medico-Legal Autopsy:
- To determine the cause of death
- To establish the manner of death (natural, accidental, suicidal, or homicidal)
- To estimate the time since death
- To collect evidence (e.g., bullets, poison, semen, injuries)
- To identify the deceased (in unknown bodies)
Who can perform the Medico-Legal Autopsy?
Eligible
| Criteria | Requirement |
|---|---|
| Medical Qualification | MBBS (minimum); MD (Forensic Medicine) preferred |
| Registration | Must be registered with Medical Council (e.g., NMC/MCI in India) |
| Posting | Must be in a government hospital or medical college |
| Legal Authorization | Must have police or magistrate’s written requisition |
| Special Training | Trained in forensic procedures (mandatory for complex/sensitive cases) |
Not Eligible:
- Private doctors or hospitals (for legal autopsies)
- Unregistered or untrained practitioners
- Homeopaths, ayurvedic, or alternate medicine doctors
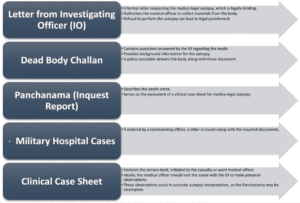
Documents pre-requisites the Medico-legal Autopsy
Dying Declaration in Medico-Legal cases
A dying declaration is a statement made by a person who is on the verge of death, explaining the cause or circumstances of their death. In medico-legal contexts, it holds exceptional evidentiary value, especially in cases involving homicide, suicide, burns, or poisoning, where the victim may not survive to testify in court.
Legal Definition (Indian Evidence Act, Section 32(1)):
“Statements made by a person as to the cause of their death or as to any of the circumstances which resulted in their death, in cases in which the cause of that person’s death comes into question, are relevant whether the person who made them was or was not, at the time when they were made, under expectation of death.”
Importance in Medico-Legal Death:
- A dying declaration can be sole basis for conviction if found trustworthy.
- Crucial in burn injury cases, domestic violence, poisoning, and assault.
- Often guides cause of death determination during autopsy.
- Medical officer may need to record or witness the declaration if a magistrate is unavailable.
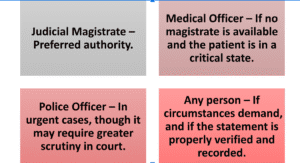
Who Can Record a Dying Declaration?
Conditions for a Valid Dying Declaration:
- The victim must be mentally fit (certified by the attending doctor).
- It must be voluntary and without coercion.
- The statement should be clear, coherent, and complete.
- If possible, it should be recorded in the victim’s own words.
- Signature or thumb impression must be taken (unless the victim is physically unable).
Role of Medical Officers in MLC Deaths:
- Certify mental and physical fitness of the patient.
- May be called to record the declaration if magistrate is not available.
- Document and preserve the declaration along with case records.
- Assist the court as an expert witness.
Supreme Court Guidelines and NHRC Recommendations
In the case Ram Bihari Yadav v. State of Bihar (1998) 4 SCC 517, The Supreme Court emphasized that postmortem reports serve as crucial corroborative evidence in criminal trials. In this case, the Court ruled that while the testimony of eyewitnesses carries primary weight, medical evidence—including postmortem reports—serves to corroborate or contradict such testimony. The Court clarified that medical evidence cannot by itself establish guilt, but it can substantially strengthen or weaken the prosecution’s case. The judgment reinforced the need for thorough and accurate medico-legal documentation, especially in homicide and suspicious death cases.
Further in the case Roopa v. State of Karnataka (2003) 1 SCC 1 The Court reaffirmed the binding nature of NHRC guidelines for conducting autopsies in custodial deaths.
In this PIL, activist Roopa challenged the lack of proper procedure in custodial death investigations in Karnataka prisons. The Supreme Court took serious note of procedural violations and strongly reiterated that all custodial deaths must be investigated following NHRC guidelines. These include:
- Videography of the entire autopsy
- Conducting autopsies by a panel of doctors
- Preserving viscera and tissue samples
- Submitting reports directly to the magistrate and NHRC
The Court ruled that non-compliance with these safeguards can lead to tampering, loss of evidence, and denial of justice, thereby mandating strict adherence.
Challenge an Autopsy Report
If the person is dissatisfy with the autopsy report then the same can be challenged by different ways. Here the legal remedies include-
- Request for Second Postmortem: Family can submit a written request to:
- The District Magistrate.
- The Superintendent of Police.
- The Court (via an advocate).
- Writ Petition: File a writ petition under Article 226 (High Court) for:
- Second post-mortem.
- Independent investigation (CBI/SIT).
- Judicial inquiry or re-autopsy under court supervision.
- Right to Information (RTI): The family can obtain:
- Post-mortem report.
- Inquest report.
- Medical treatment records.
- Human Rights Commission: A complaint can be lodged with the NHRC or SHRC in cases involving custodial or institutional negligence.
Parties Who Can Challenge an Autopsy Report
Here the person can be-
- Accused Person
- May question the accuracy or impartiality of the report to weaken the prosecution’s case.
- Can demand an independent medical review or second autopsy if foul play or manipulation is suspected.
- Victim’s Family or Legal Heirs
- Can challenge the report if they believe:
- The findings are incomplete, inaccurate, or misleading.
- There was negligence or bias by the medical officer.
- There is a cover-up, especially in cases of custodial death, political violence, or dowry death.
- May request a second autopsy (with court permission) or judicial inquiry.
- Investigating Officer (IO) or Police
- If the findings do not align with investigation or witness statements, the IO can request a re-examination, clarification, or even a second postmortem.
- Court or Magistrate
- The Magistrate or Trial Judge can:
- Question the reliability of the autopsy report.
- Order further forensic examination.
- Summon the medical officer for cross-examination.
- Approve second autopsy or independent expert review.
- Human Rights Commissions (e.g., NHRC in India)
- Can challenge or audit autopsy reports in cases of custodial deaths, encounters, or state abuse.
- May recommend re-autopsy, videography of procedures, or independent panels.
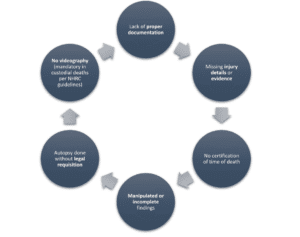
Grounds for Dissatisfaction
In the recent case V. Eswarappa v. CBI & Ors (2023), The Supreme Court allowed a second autopsy in light of allegations of a cover-up in a political leader’s suspicious death.
In this recent case involving the death of a political worker linked to a senior politician, suspicions arose regarding the accuracy and integrity of the initial autopsy. Based on public outcry and potential tampering, the Court ordered a second postmortem. The judgment emphasized that the pursuit of truth and justice overrides procedural finality, and a second autopsy is justified where there are credible doubts of foul play or medical negligence. This case reinforced the legal provision for second autopsies under compelling circumstances.
Conclusion and Recommendations
The process following a death in an MLC must be transparent, thorough, and in accordance with established legal protocols. It is critical that:
- Family members are informed of their rights.
- Second postmortem options are facilitated without delay.
- Autopsy procedures are standardized and videographed.
- Independent investigations are initiated in cases of doubt.
Strengthening procedural integrity in MLC deaths will enhance public trust in the medical-legal system and reinforce accountability.
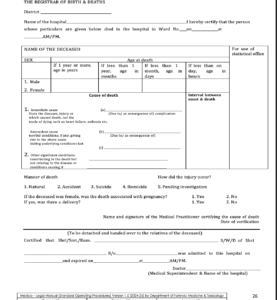
Following is the
Post-Mortem Report: Required Components
1. Basic Details
-
Name of Institution / Hospital
-
Post-Mortem Report Number
-
Name of the Doctor Conducting the Autopsy
-
Date and Time:
-
Receipt of body and inquest papers
-
Start and end time of autopsy
-
Inquest examination date and time
-
2. Case Particulars
-
Full Name of the Deceased (as per police or jail record)
-
Parent’s/Spouse’s Name
-
Address of the Deceased
-
Approximate Age and Sex
-
Name and Rank of Police Officials Who Brought the Body
-
Police Station Details
-
Identifying Persons (Name and address of relatives or known persons)
3. If Death Occurred in Hospital
-
Date & Time of Admission
-
Date & Time of Death
-
Hospital Central Registration Number
4. Alleged History
-
A brief note of the incident as per the inquest papers (e.g., suspected cause, event, or condition leading to death)
5. Observations Section
A. General Observations
-
Length and Weight of the Body
-
Physique (Lean, Medium, Obese)
-
Build (Well built, Poorly built, Emaciated)
-
Unique Identification Marks (Moles, Scars, Tattoos)
-
Fingerprints (on attached sheet)
-
Description of Clothes Worn
-
Post-mortem Changes:
-
PM staining (lividity)
-
Rigor mortis (presence and extent)
-
Decomposition, if any
-
B. External Examination
-
Condition of eyes
-
Condition of mouth, nose, ears
-
Nails
-
External injuries (number, type, size, location, age of injury, fresh or old)
Note: Use standard injury diagrams to mark injury locations.
C. Internal Examination
i. Head and Brain
-
Scalp, Skull (fractures)
-
Meninges, Cerebral Vessels
-
Brain Condition and Weight
ii. Neck
-
Tongue, Pharynx, Larynx
-
Vocal Cords
-
Neck Muscles, Cartilage
iii. Chest
-
Ribs and Chest Wall
-
Trachea, Bronchi, Oesophagus
-
Lungs (weight and condition)
-
Heart (weight and findings)
-
Diaphragm and large blood vessels
iv. Abdomen
-
Stomach (contents, smell)
-
Small & Large Intestine
-
Liver, Spleen, Kidneys, Pancreas (with weight)
-
Bladder, Urethra
-
Genital Organs (including signs of injury, semen, foetus)
v. Spine and Spinal Cord
-
To be opened if specifically indicated
vi. Any Additional Observations
6. Medical Opinion
-
Probable Time Since Death
-
Cause of Death:
-
Immediate Cause
-
Underlying or Contributory Cause
-
-
Type of Injuries: Ante-mortem or Post-mortem, with duration
-
Nature of Injuries: Accidental / Suicidal / Homicidal / Natural
-
Whether injuries were sufficient to cause death in normal course
-
Any other remarks
7. Specimens Collected
-
Viscera (liver, kidney, spleen, stomach contents, etc.)
-
Blood (liquid and dried sample)
-
Clothes of the deceased
-
Foreign bodies (bullets, ligature, etc.)
-
Slides (semen, vaginal smears, etc.)
-
Photographs or video footage (especially in custodial or encounter deaths)
-
Seal sample
-
Inquest papers (numbered and signed)
8. Handover Section
-
Details of items handed over to Investigating Officer (body, reports, samples)
-
Name, Belt No., and Police Station of I.O.
-
Signature of Receiving Officer
-
Signature and Name of Medical Officer
-
Official Stamp/Seal
Incase, You wish to discuss, and talk on any such matter that, ‘You may need help with’. Feel free to contact us. Our team at www.legalwellbeing.in shall be happy to assist.
Written by Team Member(s) and Ms. Tanishka Jain.